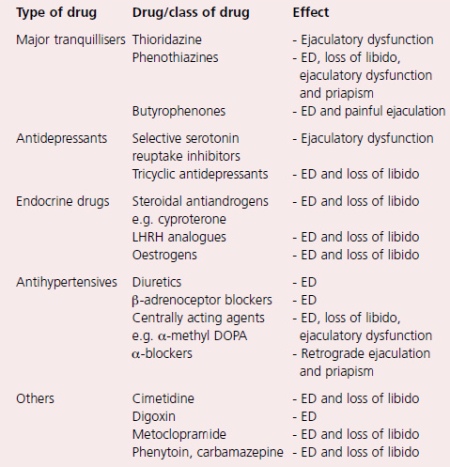
A large number of drugs can impair sexual function, either by an effect upon erectile function, ejaculatory function or sex drive. Some of the more commonly used drugs are listed in table. Use of these drugs very rarely produces ED on their own, their action usually being an adjunct to another pathophysiological mechanism.
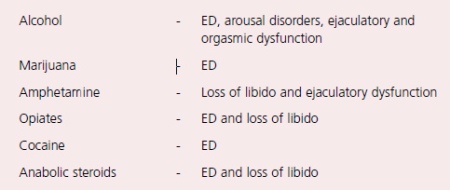
The sexual effects of recreational drugs are shown in table. Surgery and radiotherapy can also impair erectile function.
The commonest surgical cause of ED is radical pelvic surgery for rectal cancer, bladder cancer or prostate cancer. The parasympa- thetic nerves that subserve penile erection run adjacent to the prostate and are often damaged during such radical surgery. Techniques of surgery (in particular radical prostatectomy) have been devised with the aim of both nerve and potency preservation.
Other surgery that can lead to ED includes spinal surgery and surgery for Peyronie’s disease or for priapism, while radiotherapy for bladder, prostate or rectal cancer will often lead to delayed ED via a vasculogenic mechanism.
Conclusion
The pathophysiological mechanisms involved in the development of erectile dysfunction are many and varied. A number of mechanisms may be active in an individual, and nowhere is this more true than in men with diabetes. Around 50% of diabetic men can expect to develop ED, and pathophysiological mechanisms involved include peripheral autonomic neuropathy, large vessel atheroma, small vessel microangiopathy, endothelial dysfunction and psychological disorders.
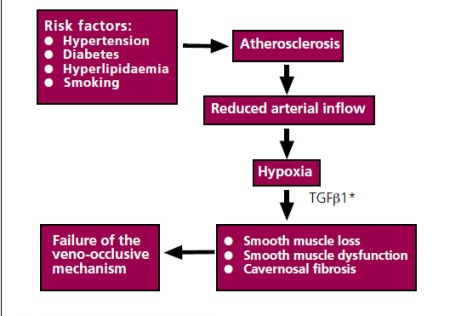
In the general population, the commonest causes of ED are vascular, and there is increasing evidence that the risk factors for atherosclerosis, namely hypertension, smoking, hyperlipidaemia and diabetes, are all strongly associated with ED.
This has two important consequences.
- Firstly, control of these risk factors might be expected to reduce the risk of ED.
- Second, when men do present with ED, it is important to identify these risk factors, not only to potentially improve the ED, but also to try to prevent other future cardiovascular sequelae.
Vascular disease is probably the most common cause of ED, and of all the vascular causes, the commonest is atherosclerosis. However, not only is atherosclerosis associated with ED, but its risk factors, namely smoking, hypertension, hyperlipidaemia and diabetes, are also associated with the development of ED. The Massachusetts Male Aging study described an association between ED and hypertension, diabetes and hypercholesterolaemia. The Cologne study of men with ED also confirmed an association between ED and diabetes and hypertension, while several studies have demonstrated an association between smoking and ED. At a cellular level, it has been suggested that a reduced arterial inflow leads to relative hypoxia within the penis with subsequent cellular effects. The crucial cellular mediator appears to be Transforming Growth Factor Beta 1 (TGF1), which is increased in hypoxia and induces trophic changes in the cavernosal smooth muscle.
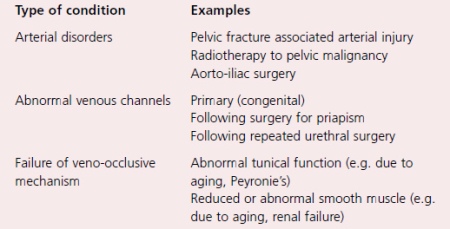
In addition to atherosclerosis, other disorders of both the arterial supply and the venous drainage of the penis can result in ED, and examples of both.
When there is failure of the veno-occlusive mechanism, the phenomenon of venous leakage occurs. This is a purely radiological phenomenon seen during specialised radiological imaging of the penis (cavernosography). When originally described, it was thought that the abnormal veins represented the primary pathological pathological abnormality, and for some years surgical ligation of these veins was undertaken as a means of treating ED. However, with the understanding that the venous leak was almost always secondary to abnormalities of the tunica albuginea or to disease of the cavernosal smooth muscle (and with the realisation that the results of venous surgery were poor), surgical treatment has almost completely disappeared.
Cellular causes of erectile dysfunction
Two types of cavernosal cells are central to penile erection; namely smooth muscle cells and endothelial cells. The vascular endothelial cells line the trabecular spaces of the cavernosal sinusoids and release a variety of vasoactive chemicals which control smooth muscle tone within the penis. The most important of these is NO. Diseases which damage the endothelium impair the vascular response of the penis to neural stimuli. A number of diseases damage the endothelium, including hypercholesterolaemia, but the most important is diabetes mellitus.
The structural changes in the endothelium that are produced by diabetes are accompanied by functional changes that result in impaired smooth muscle relaxation.
The diseases of smooth muscle that can result in erectile dysfunction have already been alluded to above. Aging results in reduced penile smooth muscle, as does atherosclerosis, while renal failure results in smooth muscle dysfunction. When the smooth muscle malfunctions, arterial dilatation is incomplete, cavernosal relaxation fails to occur and the veno-occlusive mechanism fails.
Neurogenic erectile dysfunction
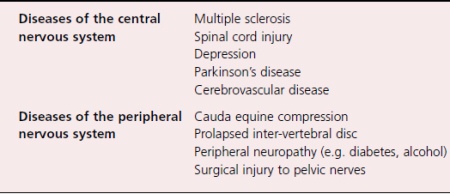
Diseases of both the central and the peripheral nervous system can result in erectile dysfunction. Again, there are too many to allow much detailed discussion and a list of the commoner neurogenic causes of ED.
Several psychiatric conditions, such as depression, can result in ED, and they are more usefully considered as organic causes rather than psychogenic. In fact, the relationship between depression and ED is a complex one. Depression can certainly result in ED, but mild depression can also result from ED, such that it has become clear that treatment of ED in men with mild depression can improve the depressive symptoms as well as the ED. A further issue is the sexual effect of the drugs used to treat depression (see later).
Spinal cord injury affects erectile function, but the picture depends upon the level and extent of the injury. Broadly speaking, men with high lesions can still get reflex erections (via intact reflex pathways) while men with low cord lesions can sometimes continue to get psychogenic erections (via intact sympathetic pathways).
Other issues that are relevant in men with neurological disease are the effects of the disease upon mobility, manual dexterity and urinary function. Disorders of one or all of these systems might also exacerbate any erectile dysfunction. Nowhere is this seen more clearly than in multiple sclerosis, where quite severe disability can be seen in young men who might have relatively normal sexual function. Furthermore, even if erectile function has been lost, but can be restored by treatment, other disabilities might preclude sexual activity.
Endocrine mechanisms of erectile dysfunction
Testosterone is central to normal male sexual function having an important role in both sexual drive and penile erection. However, a reduced level of testosterone has variable effects upon sexual function. There is reduction in libido, but a less marked effect upon erectile function. Men who are hypogonadal do not necessarily lose psychogenic and reflex erections. They do, however, have diminished nocturnal erectile activity, with both reduced duration and rigidity of the erection.
Again, there is a large number of causes of reduced serum testosterone, but they can be broadly classified into primary hypogonadism (where the disease is testicular) and hypogonadatrophic hypogonadism, where the primary disease affects the pituitary or the hypothalamus.
- Examples of the former are the hypogonadism which may follow mumps orchitis, or that which follows radiotherapy to the testes.
- Examples of the latter include congenital causes such as Kalmann’s syndrome and acquired causes such as pituitary tumours.
A rare endocrine cause of ED is a prolactin secreting tumour of the pituitary. The presenting symptoms are typically ED, galactorrhea and gynaecomastia.
The serum testosterone is usually reduced and the diagnosis is made by CT scanning of the pituitary.